Like many women and men, I found my breast tumour myself. I never did regular (or, as I have now learned, proper) self exams; I would just have a superficial feel around every couple of months and sufficiently freak myself out about all the lumps and bumps I felt to not try again for another couple of months.
My doctor told me, verbatim, that I had “won the lottery” finding my tumour when I did. Most people who discover their lumps by accident or with improper self exam technique on average find their tumours when they have reached about the size of a ping pong ball. When untrained-me discovered my lump, it was still small at about 1.1 cm, around the size that is considered the optimal standard for a trained doctor to find a lump during a clinical exam. I am on the bustier side (much more so at that time too), and so it was ONLY because the tumour was at the very outside edge of my breast tissue and close to the surface of my skin that I found it at all; I could see it with my naked eye if I pushed my skin down, but if it had been in the centre of my breast, buried under all of that tissue, it would have had to get a lot bigger before I found it since I wasn’t really checking properly. The mammogram didn’t pick it up either, even though I could literally see the lump with my own eyes when I pressed my skin down, so even if I had been at an age old enough to be getting annual mammograms, it wouldn’t have made a difference. I was definitely lucky.
But it’s a bit more than luck, because I wouldn’t have found it at all if I didn’t do even my improper and infrequent self exams. It occurred to me recently that I STILL wasn’t doing proper self exams, because I was afraid of what I might find. Sure, I felt around far more regularly, but I didn’t follow the proper techniques. Even though I have felt a cancerous tumour myself, time has a tendency to dull the sharpness of our memories, and I found that I couldn’t be sure anymore what my tumour felt like when I found it. Additionally, I didn’t really know how to tell the difference between normal, healthy, nodular breast tissue and a concerning nodule. So, I just wasn’t doing proper exams.
I came across an article recently that was discussing how routine cancer screenings have plummeted because of the coronavirus, highlighting for me that it has never been more important to learn proper technique and commit to doing regular, thorough exams. So, I decided I was going to make that commitment.
It was serendipitous that Dr. Veronique Desaulniers was hosting a webinar on breast self exams at the same time I was thinking about how I could up my self exam game. More widely called Dr. V by those who follow her work, she is a two-time breast cancer survivor and the author of “Heal Breast Cancer Naturally”. In the webinar, she covered a lot of info about the importance of regular self exams, her own history with discovering her cancer twice on her own, some of the best screening methods other than self exams, and much more as well as introduce her new breast self exam training model and video. In today’s post, I will going over my key takeaways from her webinar as well as include a video testimonial about my experience with her My Breast Friend model and self exam method.
Key Takeaways
 The Importance of Self Exams
The Importance of Self Exams
According to a study from 2001, “Despite increased use of screening mammography, a large percentage of breast cancers are detected by patients themselves” [1]. Mammograms account for 43% of detections, intentional self breast exams account for 25%, accidental self-discovery for 18%, clinical breast exams by a doctor for 13%, and 1% are detected through other methods. So, if you add together self exams and accidental discovery, self exams (whether intentional or not) account for the same percentage of breast cancer detection as mammograms, at 43% for both.
 Issues with Mammograms
Issues with Mammograms
In addition to the true importance of self exams, Dr. V also discussed some issues that exist with mammograms that are important to be aware of when determining which method of screening you want to use in alongside self exams.
Mammograms use radiation to create their images, much like an X-ray. Dr. V quoted the British Journal of Radiology in her webinar, stating: “Low energy X-ray radiation from mammograms cause DNA damage that may result in an increased risk of Breast Cancer”. Although I was unable to find that particular study, I found others that confirm it is possible to develop breast cancer from the radiation you are exposed to during mammograms, particularly if you have large breasts and more images are therefore required to complete your mammogram [2, 3]. We can extrapolate and also conclude that if more images equals a greater risk, young women who have had breast cancer and as a result are receiving regular mammograms much earlier in life (therefore receiving far more mammograms over their lifetime) will experience an increased risk as well.
Another issue Dr. V discussed was that mammograms use compression, flattening your breasts to get a clear image. In today’s mammograms, 42 pounds of pressure are applied to the breasts. Apart from being painful, this compression may rupture small tumours and blood vessels, therefore contributing to the spread malignant cancer cells throughout your body. Only 22 pounds of pressure are needed to rupture the encapsulation of a cancerous tumor (4). As almost double that is applied during a mammogram, the amount of pressure involved therefore has the potential to rupture existing tumors and spread malignant cells into the bloodstream (5; side note, this is an excellent article for anyone interested in learning more about the issues with mammography).
Finally, dense breasts, like mine and many women’s, pose problems. “Breast density is one of the strongest, if not THE strongest, predictor of the failure of mammography screening to detect cancer” [6]. You may remember me mentioning above that even though I could see my lump with my naked eye when I pressed my skin down, my mammogram was still negative because of my dense breasts. According to areyoudense.org, 2 out of 3 pre-menopausal women have dense breasts, 1 out of 4 post-menopausal women have dense breast tissue, and those with dense breasts have a risk factor 4-6 times greater of developing breast cancer because of the difficulty with detecting cancer in dense breasts on mammograms, which is the most used detection method. Dr. V shared that mammograms only detect 48% of cancers in dense breasts; less than half! So if you have dense breasts, it is actually more likely that your cancer won’t be detected by a mammogram than will.
Alternatives to Mammograms
 MRI’s
MRI’s
Benefits: MRI’s use strong magnetic fields to generate their images, so there is no radiation. There is also no compression involved, so you avoid the risk of rupture and pain that we discussed earlier. These are a good alternative as well because they are much more sensitive than mammograms and can better detect cancer, particularly in dense breasts
Issues: The downside to MRI’s is that in order to get a really clear image, they must use a contrast dye called gadolinium, which can be toxic and has a tendency to accumulate in the brain. Reported side effects include joint pain, muscle fatigue and cognitive impairment that can last for years. “The gadolinium used in the dye is anchored to a molecule to create a nontoxic compound. Scientists believed that most of the gadolinium left the body along with the nontoxic compound. But then in 2013, a radiologist in Japan reported finding differences in the brain scans of people who had multiple MRIs. Tissue and autopsy reports have also confirmed that gadolinium can accumulate in the brain and other organs” [7]. It is an option to get an MRI without the dye and many women still get a good image that way, so that’s a choice to consider. I do MRIs currently, but after this webinar, I am going to ask my oncologist if we can do ultrasounds going forward, since I will get many MRIs over my life if I stick with them and I don’t like the sounds of gadolinium toxicity.
 Ultrasound
Ultrasound
Benefits: Ultrasounds use high frequency sound waves and convert them into an image, so like MRI’s there is no radiation. They also have much better image reliability, again particularly for dense breasts, and so they make a good complement to mammography.
Why they are better, for young women in particular: As we discussed earlier, mammograms are difficult to read in young women because their breasts tend to be dense and full of milk glands. Glandular tissue looks dense and white – much like a cancerous tumour. The mammogram tech showed me my “negative” image in the room because she couldn’t see anything and she wanted to reassure me, as I’m sure she could tell I was scared; it really all looked the same. Locating an abnormality in the midst of dense gland tissue can be like finding a snowball in a snowstorm as I like to say.
Thermography
How it works: An area where cancer is growing is often inflamed, has more blood flowing to it thanks to angiogenesis (a tumour’s ability to create new blood vessels to feed it by emitting chemical signals), and has more cellular metabolic activity due to the rapid and unending replication cancer cells undergo. Inflammation + blood flow + metabolic activity = more heat, and that is what thermography takes advantage of. Thermography uses a digital infrared thermal imaging camera to pick up the heat patterns being emitted by your body. A doctor than studies the resulting image to look for asymmetrical heat patterns. Abnormal heat patterns are some of the earliest signs of developing cancer. Check out the images below that Dr. V shared of a healthy scan versus various concerning ones.
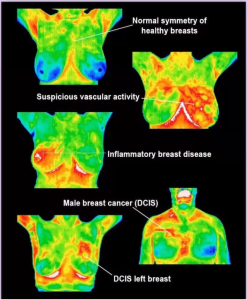 Benefits: The benefits of course are that there is no radiation used, thermography does not require gadolinium contrast dye, and there is no compression involved.
Benefits: The benefits of course are that there is no radiation used, thermography does not require gadolinium contrast dye, and there is no compression involved.
Issues: Some insurance companies may cover thermography, but you will likely have to pay out-of-pocket for it. The other issue people may have with thermography is that it is not detecting actual cancer, but rather the abnormal heat patterns that can accompany cancer growth caused by the reasons listed above. Therefore, thermography will not tell you whether you have cancer but will instead tell you when there is something concerning that requires you to go for additional screening, much like a self exam; this makes it a great complementary tool to use in between regular screenings of MRIs, ultrasounds, or mammograms to catch interval cancers. Dr. V mentioned that every woman should be using two screening methods, whether that’s mammography and thermography, or MRI and ultrasound, or MRI and mammography, or thermography and ultrasound, or any combination of these; so, thermography is a great choice for your second screening method.
Interval Cancers
A study was done on interval cancers (cancers that are detected between clinical screenings such as mammograms) to determine how many were truly interval (actually developed in the time between scans) and how many were just missed by the screening method. The study concluded that 77% of cases examined in the study were true interval cancers, developed and detected in the 1-2 year interval between screening examinations (International Journal of Cancer, July 2012, 131[2], 417-25). This means that the best chance of catching a good majority of interval cancers early (before your next screening finally rolls around) is through regular self exams.
 Detecting a Lump or Other Sign of Potential Cancer
Detecting a Lump or Other Sign of Potential Cancer
What does a breast lump feel like?
According to Dr. V, a breast lump is most likely cancerous if it is hard, is unevenly shaped, and is immobile (does not move easily under the skin), and that it may or may not be painful. Of course, a cancerous tumour can in fact be quite mobile, like mine was, and so even if what you feel doesn’t match these identifiers, still go get ANY changes looked at by your doctor. However, you first have to become very familiar with what your breasts usually feel like so that you can tell when there is a change that needs looking at.
Include a visual inspection in front of a mirror as part of your exam
Hold your arms at your sides, look front on and to the left and right. Then, place your hands on the back of your head or above your head with your palms pressed together. Look front on and to the left and right. Finally, place your hands on your hips and press down, and again look front on and to the left and right. You are looking for puckering, dimpling, or changes in size, shape or symmetry, and checking if your nipples are turned in (inverted). You should also lift your breasts to see if the ridges along the bottom are symmetrical.
Other signs to look for include skin changes, swelling or redness, pitting of the skin like the skin of an orange, visible difference in shape or size or positioning between both breasts (that isn’t normal for you), changes in appearance of nipples, nipple discharge other than breast milk, peeling or flaking of nipple skin, general pain in the breasts, itchy breasts, and swollen lymph nodes in the armpit or upper chest.
Dr. V reiterated that it is best to do a self exam in the shower or lying in bed and to do it 3-5 days after your period when your breasts aren’t as tender or naturally lumpy. She also noted that it is best to do a self exam at the same time every month, as it will give you the most accurate and consistent knowledge of what your breasts feel like normally. She also suggested keeping a log or journal of what you feel each month and to note any changes, as this way you will be far more likely to remember exactly what you feel normally and notice when there is a change.
 My Breast Friend Model and Training Method
My Breast Friend Model and Training Method
This brings us to Dr. V’s My Breast Friend training model and exam method. Decades ago, a group of scientists at the University of Florida, with the support of The National Cancer Institute and the National Science Foundation, developed a silicone breast training model. The result was The MammaCare Method, which is the recognized gold standard for performing and teaching clinical and personal breast exams and that has trained thousands of doctors around the globe for over 30 years on what to feel for during an exam of a patient.
Learning this method for performing breast exams may just save your life, with one study concluding that the performance of specific Breast Self-Exam may reduce the risk of death from breast cancer [8]. Couple this with the results of a 25-year study that concluded “Annual mammography in women aged 40-59 does not reduce mortality from breast cancer beyond that of physical examination or usual care […]” [9], and proper physical self exams begin to emerge as more and more important.
Dr. V’s My Breast Friend is a simulation model based on the same silicone training model used with The MammaCare Method. It provides proper training for your fingers with a life-like breast exam model and tumours modelled after real tumours removed from patients. There is an accompanying training video based on the The MammaCare Method that teaches you the technique for a truly thorough and proper breast self exam, the training for which includes three important steps:
- Your fingers must be taught what to feel for, which can only be done with an accurate breast model.
- You must be taught where to feel; the educated and trained fingers must be brought into contact with all breast tissue, which many people don’t realize actually extends from underneath your breast all the way up to your collarbone and over into your armpit to include the lymph nodes that are in those two areas. You can see a diagram in the “About” section of the My Breast Friend website, but you should be moving from outside to inside, moving all the way down, and then over one finger width towards the centre of your chest before moving back up, over one finger width, then down, and so on until you reach the centre of your chest. You then repeat that on the opposite side (it’s much easier to grasp while watching the video, I promise!).
- You must be taught how to feel; the fingers must use the correct pressure – light, medium, and deep to your chest wall – and you must use the correct part of your fingers to feel – the pads and not the tips! You should be making small circular motions at each of the three levels of pressure before moving your fingers to the next point.
Dr. V emphasized that even if you have had a double mastectomy, it is important to continue to do self exams. She spoke about tumours returning around incision scars and even hiding under scar tissue; this coupled with the fact that your breast tissue actually extends so far up your chest makes it important to become familiar with your new terrain after surgery and to look for changes through regular self exams.
But how to properly do these exams? There are so many pointers and instructions online, it can be overwhelming and frustrating. And even with clear written instructions on how to do a proper exam, it doesn’t help if your fingers can’t really tell the difference between your normal nodular tissue and something that is potentially concerning. A study on how best to teach self exams to women concluded that Mammacare Method instruction, which the My Breast Friend technique employs, resulted in more long-term improved lump detection and better examination technique than did traditional instruction or physician encouragement. It also concluded that breast self-examination instruction should emphasize lump detection skills (i.e. what to feel for and how to know when you should go to your doctor) [10], which the My Breast Friend model absolutely does. And there has never been a better time to learn this skill, while so many are stuck at home and unable to get their regular screening due to COVID-19.
If you aren’t sure whether My Breast Friend is right for you, please take some time to watch my review and testimonial below. I go into detail about my experience using the model and training video for the first time, what I loved, what I think needs to be improved, and my overall recommendations for it. Spoiler, I really love this model and believe in its benefits. Watch to find out why!
I’m sure that many of you feel intimidated about starting to do regular self exams; I know I was. Like me, you likely feel that you don’t know what you are feeling for, and so you freak yourself out every time you do a self exam. You feel like your breasts are always lumpy, and so you are scared to touch them in this way in case you find something and don’t know whether to be concerned about it or not.
Dr. V’s webinar was a big wake up call for me. As she said, it’s time to get over it! Ignorance is NOT bliss and size matters. When cancer is small, less than 1cm (pea sized) and has not spread, the patient’s 15-year survival exceeds 88%. And the best way to find it when it is small, especially if you are young, is to do regular self exams.
The good news is that 8/10 lumps are NOT cancerous, but if you do find anything unusual, any changes at all, see your doctor immediately. My doctor told me after I was diagnosed that she has patients come in with golf-ball-sized lumps, and she’ll ask how long they have felt them for and they say 6 months or more. She expressed so much frustration at this, and it really highlighted for me back then that time makes all the difference. You will have to deal with it eventually, it will become unavoidable, so wouldn’t you rather deal with it when it is 1cm instead of 5cm and spreading? Don’t wait! Commit to doing self exams regularly and doing them the right way. To learn more about My Breast Friend and to get your own, visit their website here.
Happy Healing ❤️
References
- Self-detection remains a key method of breast cancer detection for U.S. women. – https://www.ncbi.nlm.nih.gov/pubmed/21675875
- Enhanced biological effectiveness of low energy X-rays and implications for the UK breast screening programme. – https://www.ncbi.nlm.nih.gov/pubmed/16498030
- Radiation-Induced Breast Cancer Incidence and Mortality From Digital Mammography Screening: A Modeling Study. – https://www.ncbi.nlm.nih.gov/pubmed/26756460
- A Comparative Review of Thermography as a Breast Cancer Screening Technique – https://journals.sagepub.com/doi/pdf/10.1177/1534735408326171
- Mammography Controversies: Time for Informed Consent? JNCI: Journal of the National Cancer Institute – https://academic.oup.com/jnci/article/89/15/1164/2526360
- Breast density as a predictor of mammographic detection: comparison of interval- and screen-detected cancers. – https://www.ncbi.nlm.nih.gov/pubmed/10880551
- Concerns Raised About MRI Contrast Dye – https://www.cancertodaymag.org/Pages/Summer2019/Concerns-Raised-About-MRI-Contrast-Dye.aspx
- Effect of breast self-examination techniques on the risk of death from breast cancer – https://www.researchgate.net/publication/13867503_Effect_of_breast_self-examination_techniques_on_the_risk_of_death_from_breast_cancer
- Twenty five year follow-up for breast cancer incidence and mortality of the Canadian National Breast Screening Study: randomised screening trial – https://www.bmj.com/content/348/bmj.g366
- How best to teach women breast self-examination. A randomized controlled trial. – https://www.ncbi.nlm.nih.gov/pubmed/2184711




0 Comments